The Ultimate Guide to Choosing an Oxygen Concentrator in Australia
For individuals living with chronic respiratory conditions, maintaining independence while managing oxygen therapy is a top priority. Whether you are navigating the bustling streets of Sydney or enjoying the coastal breeze of New South Wales, understanding how to select the right oxygen concentrator is essential for your health and mobility.
An oxygen concentrator is a medical device that filters ambient air to provide a concentrated flow of oxygen. Unlike traditional oxygen tanks, which have a finite supply and require frequent refills, these machines generate oxygen continuously as long as they have a power source.
This guide provides a deep dive into the technology, benefits, and practical steps for Sydney residents looking to buy or rent these life-changing devices.
What is an Oxygen Concentrator and How Does It Work?
At its core, an oxygen concentrator is an advanced filtration system. The air we breathe consists of approximately 21% oxygen, 78% nitrogen, and 1% other gases. The machine pulls in this room air, compresses it, and uses a molecular sieve to remove the nitrogen.
The Science of Oxygen Concentration
The device operates through a process called Pressure Swing Adsorption (PSA).
- Air Intake: The machine draws in air from the surrounding environment.
- Compression: An internal compressor increases the air pressure.
- Filtration: The pressurized air passes through zeolite “sieve beds” which trap nitrogen molecules.
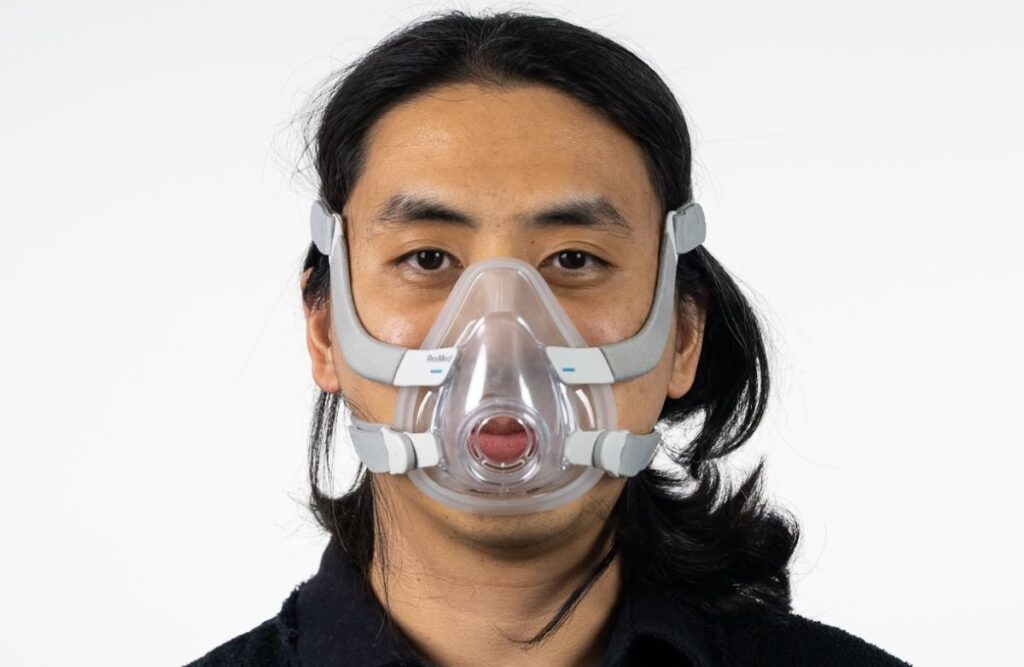
- Delivery: The purified oxygen (usually 90–95% purity) is delivered to the user via a nasal cannula or mask.
- Purge: The trapped nitrogen is released back into the atmosphere, and the cycle repeats.
Stationary vs. Portable Oxygen Concentrator Machines
When researching where can i buy or rent a portable oxygen concentrator machine, it is vital to understand the two primary categories available on the Australian market.
1. Stationary (Home) Concentrators
These are larger units designed for 24/7 use at home. They typically offer higher flow rates (up to 5 or 10 liters per minute) and run exclusively on AC power.
- Best for: Sleep apnea, COPD patients requiring high flow, and overnight therapy.
- Pros: High output, lower maintenance, cost-effective for long-term use.
2. Portable Oxygen Concentrators (POCs)
POCs are lightweight, battery-operated devices designed for active lifestyles. They allow users to travel, shop, and visit family without being tethered to a home unit.
- Best for: Travel, outdoor activities, and short errands.
- Pros: Lightweight (often under 2.5kg), FAA-approved for flights, and compact.
| Feature | Stationary Unit | Portable Unit (POC) |
| Primary Power | Wall Outlet (AC) | Battery / DC (Car) |
| Weight | 13kg – 25kg | 1.5kg – 8kg |
| Oxygen Delivery | Continuous Flow | Pulse Dose (mostly) |
| Portability | Limited (Wheels) | High (Shoulder Bag) |
Export to Sheets
Benefits of Using an Oxygen Concentrator
Transitioning from compressed gas cylinders to a concentrator offers several physiological and lifestyle advantages.
- Continuous Supply: You never have to worry about “running out” of oxygen or waiting for a delivery driver to swap cylinders.
- Enhanced Mobility: Portable models empower users to maintain their social lives and travel across Australia or internationally.
- Safety: Concentrators do not store high-pressure gas, significantly reducing the risk of leaks or fire hazards compared to traditional tanks.
- Cost-Efficiency: While the upfront cost is higher, the long-term savings on refills and delivery fees are substantial.
Real-World Use Cases: Living in Sydney with Oxygen

Managing the Sydney Commute
For a resident in the Inner West or North Shore, using a POC means you can comfortably take the ferry across Sydney Harbour or use the Sydney Trains network. Modern POCs fit discreetly under a seat and provide enough battery life for a full day out.
High-Altitude Travel
If you are planning a trip to the Blue Mountains or flying out of Sydney Kingsford Smith Airport, a POC is essential. Most major airlines allow specific FAA-approved models, ensuring your oxygen levels remain stable during cabin pressure changes.
How to Choose the Right Machine: A Step-by-Step Framework
Selecting an oxygen concentrator is a clinical decision that should be made in consultation with a respiratory specialist. Follow these steps:
Step 1: Confirm Your Prescription
Your doctor will specify your required flow rate (Liters Per Minute) and whether you need Continuous Flow or Pulse Dose. Pulse dose delivers oxygen only when you inhale, whereas continuous flow provides a steady stream regardless of your breathing pattern.
Step 2: Evaluate Your Activity Level
If you rarely leave the house, a stationary unit is sufficient. However, if you enjoy walking through the Royal Botanic Garden or traveling, a POC with a “Pulse Dose” setting is more practical.
Step 3: Check Battery Life and Power Options
Look for machines that offer “External Battery” options. In Australia, ensure the device is compatible with 240V AC power and includes a 12V DC adapter for use in cars or caravans.
Step 4: Noise Level and Size
For home use, noise (measured in decibels) is a major factor. Look for units rated under 45 dBA to ensure a quiet environment for sleeping.
Where Can I Buy or Rent a Portable Oxygen Concentrator Machine?
If you are located in Sydney or wider Australia, you have several reputable options for sourcing equipment.
Buying vs. Renting
- Buying: Best for long-term chronic conditions (COPD, Interstitial Lung Disease). It offers the lowest cost-per-year and the convenience of ownership.
- Renting: Ideal for short-term recovery after surgery, palliative care, or testing a specific model before committing to a purchase.
Sourcing in Sydney
- Specialist Medical Suppliers: Look for providers in medical hubs like Westmead, Randwick, or Kogarah. These suppliers often provide in-person fittings and demonstrations.
- Online National Retailers: Many Australian companies offer overnight shipping to Sydney and provide comprehensive warranties and local service centers.
- Hire Services: Short-term hire is readily available for travelers visiting Sydney who do not want to transport their own heavy equipment.
Internal Linking Suggestions:
- Anchor Text: “portable oxygen concentrator rental Sydney”
- Anchor Text: “best home oxygen concentrators for COPD”
- Anchor Text: “oxygen concentrator maintenance tips”
Common Mistakes to Avoid
- Buying Without a Prescription: Oxygen is a drug. Using it without professional guidance can lead to oxygen toxicity or under-treatment.
- Ignoring Sieve Bed Longevity: Sieve beds are a consumable part. Ensure the model you buy allows for easy replacement of these filters.
- Overlooking the Weight: A machine that feels light for five minutes might feel heavy after an hour. Always check the total weight including the battery.
- Purchasing from Unverified Overseas Sellers: Ensure your device is TGA (Therapeutic Goods Administration) approved for use in Australia to guarantee safety and after-sales support.
Frequently Asked Questions (FAQ)
1. Does Medicare or the NDIS cover oxygen concentrators in Australia?
Yes, depending on your clinical needs and eligibility. The NDIS may fund a concentrator if it is deemed “reasonable and necessary” for your disability. Many state-based programs (like the NSW Spectacles and Aids Program) also offer assistance.
2. Can I use a portable oxygen concentrator on a plane?
Most POCs are FAA-approved. However, you must notify your airline at least 48 hours in advance and usually carry enough battery life to cover 150% of your flight duration.
3. How long do the batteries last on a portable unit?
Battery life varies by flow setting. On a low setting (Pulse 1 or 2), many modern POCs can last 4 to 8 hours on a single charge.
4. Do I need to refill an oxygen concentrator?
No. Unlike oxygen tanks, concentrators do not store oxygen. They produce it from the surrounding air, so they never need refilling.
5. How often do I need to clean the filters?
Most machines have a gross particle filter that should be washed with warm soapy water once a week. The internal HEPA filters are usually replaced during annual servicing.
Conclusion: Take Control of Your Respiratory Health
Choosing the right oxygen concentrator is a significant step toward reclaiming your independence. By understanding the difference between stationary and portable models, and knowing where to buy or rent a portable oxygen concentrator machine in Sydney, you can ensure your therapy fits your lifestyle—not the other way around.