Sleep plays a vital role in our overall health and well-being. It is during sleep that our body repairs and rejuvenates itself, helping to maintain physical and mental health. However, for some individuals, getting a good night’s sleep can be a struggle. This is where a sleep test can help diagnose underlying sleep disorders and provide a pathway towards better sleep quality. In this article, we will explore the various aspects of a sleep test, including its importance, types, process, and most importantly, the cost involved. Understanding the cost of a sleep test is essential for budgeting and ensuring that everyone can access the sleep care they need.
The Importance of Sleep for Health
When it comes to health, sleep is often underrated. Inadequate sleep can lead to a wide range of physical, mental, and emotional health problems. Research has shown that insufficient sleep can increase the risk of chronic conditions such as obesity, diabetes, cardiovascular disease, and even certain types of cancer. Sleep deprivation can also impair cognitive function, affect mood regulation, and lower our immune system’s effectiveness. Recognizing the importance of sleep is the first step in taking control of our overall health in the sleep test cost.
Furthermore, the quality of sleep is just as important as the quantity. Deep, restorative sleep is essential for the body to undergo essential repair processes, consolidate memories, and regulate various bodily functions. This is why creating a sleep-conducive environment and practicing good sleep hygiene habits are crucial for maximizing the benefits of sleep on our health. You can visit https://hematologyjournal.net/navigating-medicare-for-sleep-apnea-test-coverage-and-options to get about medicare coverage and options for sleep apnea test .
The Role of Sleep in Physical Health
During sleep, our body repairs damaged tissues, restores energy levels, and regulates hormone production. This regeneration process is crucial for maintaining optimal physical health. Lack of sleep can disrupt these restorative functions, leading to imbalances that can compromise our overall well-being.
Moreover, sleep plays a vital role in weight management and metabolism. Insufficient sleep can disrupt the balance of hunger hormones, leading to increased appetite and a higher likelihood of weight gain. By prioritizing adequate sleep, individuals can support their efforts to maintain a healthy weight and reduce the risk of obesity-related health issues.
The Impact of Sleep on Mental Well-being
Sleep plays a significant role in mental health as well. Sufficient sleep helps to regulate emotions, improve concentration, and enhance memory and cognitive function. On the other hand, sleep deficiency can lead to mood swings, irritability, difficulty concentrating, and poor decision-making. Adequate sleep is essential for maintaining mental well-being and overall cognitive performance.
Furthermore, deep sleep stages are crucial for processing emotions and dealing with stress. By allowing the brain to go through these essential stages of sleep, individuals can better cope with daily challenges, regulate their emotional responses, and maintain a positive outlook on life. Prioritizing sleep as a key component of mental health care can lead to improved resilience and overall well-being.

What is a Sleep Test?
A sleep test, also known as a polysomnography, is a diagnostic procedure conducted to evaluate and diagnose sleep disorders. It involves monitoring various body functions during sleep, such as brain activity, eye movements, heart rate, breathing patterns, and oxygen levels. This comprehensive assessment provides valuable insights into the nature and severity of sleep disturbances, helping healthcare professionals tailor appropriate treatment plans. Learn more about polysomnography click here
During a sleep test, highly trained sleep technologists work diligently to ensure accurate and reliable data collection. They meticulously place electrodes and sensors on the patient’s body to monitor specific physiological parameters. These electrodes are carefully attached to the scalp to measure brain activity, allowing clinicians to observe the different stages of sleep, including rapid eye movement (REM) sleep and non-REM sleep. Additionally, sensors are placed near the eyes to detect eye movements, providing further information about sleep patterns.
Types of Sleep Tests
There are different types of sleep tests available, depending on the specific sleep disorder being investigated. Some common types include overnight sleep studies conducted in a sleep laboratory, home sleep tests that can be done in the comfort of one’s own bed, and daytime multiple sleep latency tests for assessing excessive daytime sleepiness. The choice of sleep test depends on factors such as the suspected sleep disorder, convenience, and cost considerations.
Overnight sleep studies conducted in a sleep laboratory offer a controlled environment where sleep technologists can closely monitor the patient’s sleep patterns. The sleep laboratory is designed to resemble a comfortable bedroom, ensuring that patients can relax and sleep as naturally as possible. The data collected during these studies provides a comprehensive assessment of sleep architecture, allowing healthcare professionals to identify specific sleep disorders, such as sleep apnea, narcolepsy, or restless legs syndrome. Learn more about it click here
The Process of a Sleep Test
The process of a sleep test typically involves spending a night in a sleep laboratory or using portable equipment at home. In a sleep laboratory, electrodes and sensors are attached to various parts of the body to monitor brain activity, eye movements, muscle tone, heart rate, and respiration. These measurements help clinicians identify any abnormalities during sleep. Home sleep tests involve wearing a portable device that records similar data but in a more convenient and less controlled environment. The collected data is then analyzed by sleep specialists to determine the presence and severity of sleep disorders.
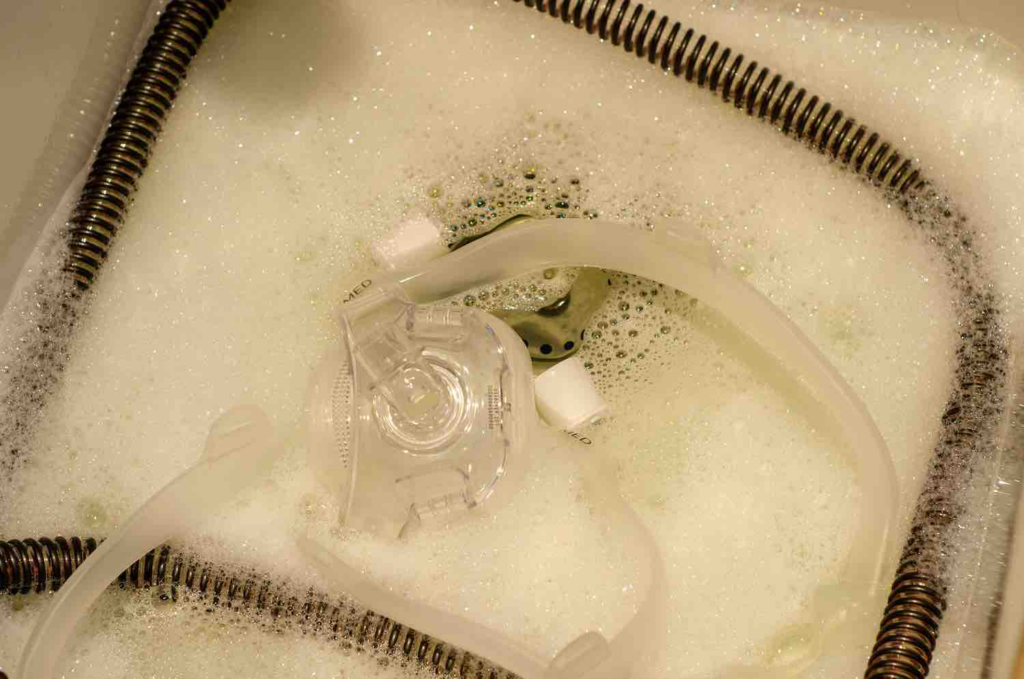
Once the sleep test is completed, the collected data is carefully analyzed by sleep specialists. They meticulously review the recorded information, paying close attention to any irregularities or abnormalities. This analysis allows them to make an accurate diagnosis and develop a personalized treatment plan tailored to the patient’s specific needs. The treatment plan may include lifestyle modifications, medication, or the use of continuous positive airway pressure (CPAP) devices to improve breathing during sleep. Learn more at https://www.mayoclinic.org/diseases-conditions/sleep-apnea/in-depth/cpap-masks/art-20546828
In conclusion, sleep tests play a crucial role in diagnosing and understanding sleep disorders. By monitoring various physiological parameters during sleep, healthcare professionals can gain valuable insights into the nature and severity of sleep disturbances. This knowledge enables them to provide effective treatment options and improve the overall quality of life for individuals suffering from sleep disorders.

Breaking Down the Cost of a Sleep Test
When considering a sleep test, it is essential to understand the different cost components involved.
Professional Fees Involved
The professional fees typically cover the expertise and time of the sleep specialist, as well as the analysis of the sleep test results. Depending on the healthcare provider and the complexity of the sleep test, these fees can vary. It is advisable to check with the sleep clinic or hospital to understand the charges and coverage, if any.
Equipment and Facility Costs
Sleep tests involve the use of specialized equipment and facilities. The cost of these resources, including the sensors, electrodes, monitoring devices, and sleep laboratory or portable equipment, can contribute significantly to the overall cost of the test. Understanding these expenses is essential for budgeting and assessing the financial feasibility of undergoing a sleep test.
Insurance and Sleep Tests
Insurance coverage can play a crucial role in managing the cost of a sleep test. It is important to understand your coverage and the specific sleep test services included in your insurance plan. Some insurance plans may cover a portion or all of the sleep test expenses, depending on the type of coverage and the diagnosed sleep disorder. Contacting your insurance provider or reviewing your policy documents can provide valuable information about the extent of coverage.
Understanding Your Coverage
Before a sleep test, it is advisable to contact your insurance provider to understand the coverage details and any pre-authorization requirements. Some sleep clinics or hospitals may have dedicated staff who can assist in verifying insurance coverage and helping navigate the financial aspects of a sleep test. Being aware of your insurance coverage can help you make informed decisions and plan your budget effectively.
Out-of-Pocket Expenses
Even with insurance coverage, there may still be out-of-pocket expenses associated with a sleep test. These can include deductibles, co-pays, or costs related to specific services or equipment that are not covered by your insurance provider. It is important to review your insurance policy and consult with the sleep clinic or hospital to estimate the potential out-of-pocket expenses.
Alternatives to Traditional Sleep Tests
For individuals who are unable to undergo traditional sleep tests due to financial constraints or other reasons, there are alternative options available.
Home Sleep Tests
Home sleep tests offer a convenient and cost-effective alternative to traditional sleep studies conducted in sleep laboratories. These tests involve the use of portable devices that can be worn at home. While they may not provide the same comprehensive data as laboratory tests, home sleep tests can still provide valuable insights into sleep quality and the presence of certain sleep disorders, such as sleep apnea.
Online Sleep Assessment Tools
Another alternative is the use of online sleep assessment tools. These interactive platforms allow individuals to answer a series of questions regarding their sleep patterns, habits, and symptoms. Based on the responses, these tools can provide an initial assessment of potential sleep problems and suggestions for further evaluation or intervention. While online assessment tools are not a replacement for professional sleep tests, they can be a starting point for individuals looking to gain a better understanding of their sleep health.
Understanding the cost of a sleep test is crucial for budgeting and better sleep management. By recognizing the importance of sleep, knowing the different types and processes of sleep tests, and understanding insurance coverage and alternatives, individuals can make informed decisions about their sleep care. Prioritizing sleep health and allocating resources towards sleep tests can pave the way for better sleep quality, improved overall health, and a well-rested future.